Stevens-Johnson Syndrome is a rare condition that effects the skin, eyes, mouth, and genitals. This condition is commonly connected to medications and/or viral infections. So, if a person with SJS acquires an ear infection, COVID or the flu, they cannot take antibiotics or NSAIDS (Non-steroidal anti-inflammatory drugs), such as ibuprofen because their bodies have an extreme, allergic reaction to these drugs. Other medications can be harmful to SJS survivors, so it is important that they keep track of prescriptions and drugs taken throughout their lifetime. Because SJS patients have different reactions to medications, treating the condition is complex. So, when an SJS patient is admitted to the hospital, doctors view each case based on the patient’s medical history, collect blood and urine tests, conduct biopsies, and then conduct further research to treat the symptoms (as quickly as they can).
Dr. Lilia Correa a Board Certified Internist who specializes in dermatology and is a professor at the University of South Florida is familiar with SJS; Correa also works at Tampa General and works with skin cancer patients.
She has worked with SJS patients for 15 years and has seen the treatment for the disorder evolve, but cases are still challenging. Correa shares, “We have TNF alpha, but it’s not a miracle because some of the patients don’t do well, but it definitely has been a game changer. It’s very important for patients to go to a high-volume center because we have specific protocols for treatments and special doctors who are familiar with SJS; the patient’s progress can change minute-by-minute.”
SJS patients will have flare-ups that could be mild or extreme, leading to a doctor visit, a lengthy stay at the hospital, or possibly death. It is important to have a team of experts beyond the emergency physician (plastic surgeons, dermatologists, ophthalmologists, immunologists, and pulmonologists) who understand this disorder, and these teams are typically stationed in burn units in major hospitals such as Tampa General.
Justin Feuerherdt, an 11-year-old, had his first SJS flare-up back in October 2022, but doctors at the hospital– without the proper protocol and understanding of SJS– had misdiagnosed the disorder as stomatitis.
In 2022, his symptoms began with fever, chills, cough, and a sore throat; it appeared he had the flu. However, the extreme pain and sores in his mouth, gums, lips, throat, and genitals did not make sense.


Justin’s records showed his allergies to penicillin and amoxicillin since age 5, so other remedies were needed to treat these symptoms. Within 3 weeks of rest at home, magic mouthwash, and ointments, the illness went away, but it returned in October 2023.
This time, the symptoms were more severe –not only affecting his mouth, throat, and genitals, but also affecting his eyes, lungs, and 5% of his skin.

Dr. Ann Lin, a professor at the University of South Florida, who specializes in dermatology and treats SJS patients at Tampa General, tended to Justin while he was hospitalized.
Lin reiterates that SJS is rare, but the approach to this condition should be multidisciplinary—meaning different specialists should be available to treat multiple factors that include the eyes and skin.
Dr. Lin continues: “Plastic surgeons will tend to the blistering or sloughing of the skin by utilizing specialized dressing. These patients can overturn overnight, and when their skin is opened, they are susceptible to infections.”
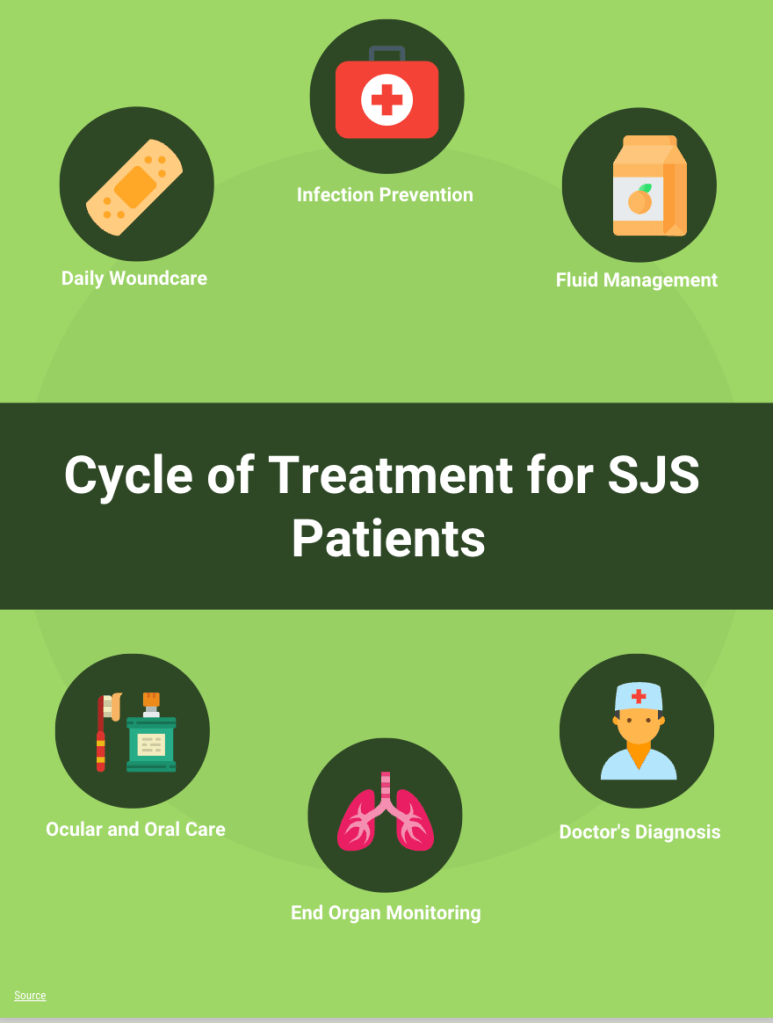
According to Deepak K. Ozhathil and Carter M. Powell, “Patients who have SJS follow a cycle of treatment when being admitted to the burn unit: daily wound care, infection prevention, fluid and electrolyte management, ocular and oral care, and end-organ monitoring.”
This cycle was followed for Justin’s condition this past October, and although his blisters stopped spreading throughout his body, he still suffered a lot of pain.
Based on trends and a consensus of data from colleagues and peers in her field, Dr. Lin decided to treat Justin with an Enbrel shot which alleviated the pain and helped his body heal.
She states, “We did a comparison of studies and went by the guidelines. There’s a newer study showing that TNF– when these patients get treatment with TNF alpha inhibitors such as Enbrel, they have shorter hospital stays and they have better prognoses. And of course, it’s not 100% because basically your immune system is very dysregulated, and there’s an inflammatory cascade, and it’s very difficult to stop it.”